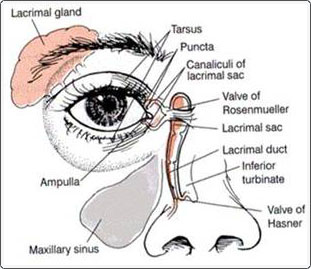
A diagram of how the nose and lacrimal system are connected.
Infants with a nasolacrimal duct obstruction present with a watery eye and an increased tear lake, mattering of the eyelashes, and mucus in the nasal corner of the eyelids. Congenital nasolacrimal duct obstruction is common and occurs in 1 to 5% of the population, with approximately 1/3 occurring in both eyes. If left untreated, approximately half of the cases will spontaneously open up by 6 months of age. After 13 months of age, the incidence of spontaneous resolution decreases to only 15%.
Management of NLD Obstruction
Significant controversy exists regarding the best timing for initial nasolacrimal duct probing. Some advocate probing even at a few months of age and suggest that it should be done in the office without anesthesia. Most pediatric ophthalmologists, however, suggest waiting until the child is at least 6 months of age, since almost half the children will have spontaneous resolution by then. Others suggest waiting until 1 or 2 years of age or longer before probing.
Medical Management
Medical management during the observational period is a combination of nasolacrimal sac massage and intermittent topical antibiotics. Some suggest massaging down towards the nose to push the tears out the nasolacrimal duct, while others suggest massaging superiorly so the material exits the punctum. This author suggests using both methods. The initial massage is directed inferiorly to push the tears in the normal direction out the nasolacrimal duct. Additional massage is directed superiorly, so that any tears that did not exit are at least cleared from the punctum. On occasion, inferior pressure itself will open a mild nasolacrimal duct obstruction. The use of topical antibiotic drops or ointments is indicated if there are signs of infection, such as mucopurulent discharge.
Surgical Management – Nasolacrimal Duct Probing
For a normal obstruction, probing is a simple but delicate procedure. Under local or general anesthesia, a small steel wire is passed through the punctum into the nasolacrimal system, through Hasner’s valve, and down out the nose. In some cases, the inferior turbinate (tiny bone in the nose) is fractured to relieve crowding. This does not hurt, nor does it create any problem in the nose. The success rate for a single nasolacrimal duct probing is approximately 90%. In cases where nasolacrimal duct probing fails, intubation with silicone tubes is indicated to establish a working system. Once inserted, the tubes are left in place for 1-3 months. Afterwards, the tubes can be removed in the office with local anesthesia. In general, silicone tubes are only used for patients who have failed the probing procedure and tearing persists. Occasionally, probing and silicone tube placement does not resolve the symptoms associated with a nasolacrimal duct obstruction. Some patients will need to undergo infracture of the inferior turbinate, a small bony area that does not open at birth. This is done during a probing procedure and does not cause any pain or discomfort when the anesthesia wears off.

Nasolacrimal duct obstruction, right eye. Note the build-up of tears and mucous along the lower lid margin. Patient also has pseudo-esotropia, as the left eye looks to be crossing, but it is really straight by corneal light reflex testing.
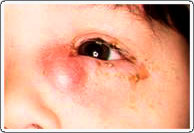
Infected nasolacrimal duct (amniotocele) requiring urgent probing and antibiotics.
In some cases, most often right after birth, the tear duct becomes infected and pus builds up under the skin (amniotocele). These patients require urgent nasolacrimal duct probing with a prompt course of antibiotics.

